At this point, it’s a given that birthing a child is painful. That the physical recovery is tough. That, sure, babies are soft and cuddly, but the parent’s body just needs a break, preferably a long one. What’s not a given: that their mind may also need some time and, crucially, some help.
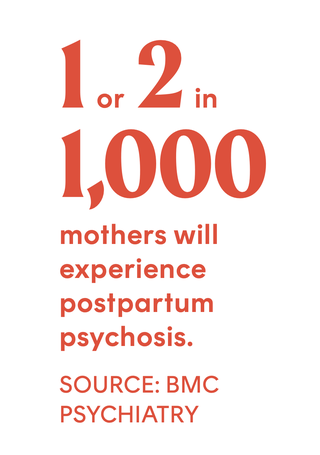
It’s not that absolutely no one is talking about maternal mental health—influential women like Chrissy Teigen and Adele have publicly shared their struggles with postpartum depression and anxiety, opening the door for countless others to do the same. (And there are countless others: Around 1 in 5 mothers will experience a mental health condition during pregnancy or in the year afterward, according to the World Health Organization.) But when it comes to one of the most severe mental health conditions associated with pregnancy and birth, there’s mostly just a lot of silence and shame, leaving vulnerable families scared and alone.
What Everyone (No, Like, Everyone ) Should Know
Postpartum psychosis, or PPP, is a mood disorder that causes new mothers to experience breaks from reality, with symptoms like delusions, hallucinations, paranoia, and sleep deprivation occurring in the days or weeks after giving birth. While there’s no clear cause, researchers believe having a personal or family history of bipolar 1 or schizo affective disorder or a prior case of PPP are the most important risk factors. But even people who’ve always had a clean bill of physical and emotional health can be impacted, says Kristina Dulaney, founder of Cherished Mom, a nonprofit promoting awareness and support for maternal mood disorders. That’s exactly what happened to her soon after the birth of her second child.
Dulaney, a nurse, never saw it coming. Neither did her doctors or family members, until the day she suddenly quit her job, believing Jesus needed her to prepare her kids for his return. Her husband called 911 after Dulaney grabbed the children while they were napping, yelling, “Please save us.” She spent the next months in inpatient and then outpatient care. Not every patient experiences religious delusions. PPP can present differently in everyone, which—along with a general lack of awareness—is one of the reasons it can be so difficult to diagnose. Michele Davidson, herself a midwife, became obsessed with the idea that her doctors caused her newborn son’s cerebral palsy. After months of being misdiagnosed with depression, she was sent to the ER, where she began hearing voices. She was admitted to a long-term care facility shortly after.
Without highly effective treatment—most often in the form of inpatient hospitalization, antipsychotic medication, and therapy—PPP will get worse. (It’s a fact that’s worth repeating: PPP does not go away on its own.) Sufferers continue to lose touch with reality, often becoming a danger to themselves and their loved ones.
This is where the news headlines come in: horrific stories about mothers murdering their babies, under the influence of psychosis. “Clinicians consider PPP to be a true psychiatric emergency,” stresses Lauren M. Osborne, MD, a reproductive psychiatrist at New York–Presbyterian/Weill Cornell Medicine. Not everyone diagnosed with PPP will experience violent delusions, but without quick and proper care, approximately 4 percent of sufferers commit infanticide. Five percent commit suicide. With that quick and proper care though, most women will make a full recovery.
Your Best Advocate Is...You
If you’re thinking about having a kid, start by understanding your own risk factors and the symptoms to look out for, and prepare your loved ones accordingly, says psychiatrist Sue Varma, MD. “In the midst of PPP,” she adds, “you’re not going to want to get help.”
Write out a plan of action with your doctor and family, especially if you’re at risk, in case PPP does arise, advises Wendy Davis, PhD, executive director of Postpartum Support International (PSI). Groups like PSI—which connects new families with trained providers, free counseling, and other resources—can help those who don’t have a built-in support system.
And keep the advocacy going by spreading the word. In our current frustrating reality, in which women already don’t always have total control over their own bodies, PPP isn’t a legislative or research priority, says Dr. Varma. “We just don’t have services in place that value women and families like other countries do.” Dr. Osborne agrees: “We need so much more education. Not only is the general public uninformed on the condition, most medical, legal, and law enforcement professionals are too.” Ob-gyns and psychiatrists have only recently started getting training in reproductive psychiatry, and our legal system doesn’t take it into consideration when sentencing, she says. Until all of this changes, the best option is to make sure anyone giving birth in your life feels supported and able to recover—both physically and mentally.
The National Maternal Mental Health Hotline offers free confidential support 24/7 in English and Spanish. Call or text 833-852-6262.
Hannah Chubb is the associate lifestyle editor at Cosmopolitan, covering all things home, travel, food, health, career, and more. She spends pretty much every hour of every day curating the internet for the best new products, trends, and travel destinations. You can typically find her looking for houses she can’t afford on Zillow or Airbnb, planning her next meal before she gets to the restaurant, or taking all of the Justin Bieber classes over and over and over again on Peloton. Follow her on Instagram.